After a few hours of monitoring, it was agreed that Billy needed to stay in until the team could reduce the swelling within his stomach.
A porter came to collect us and we started to walk through a series of corridors from A&E to the main hospital, if you had asked me to find my way back, I doubt I could mirror the journey.
After a while we entered the porters lift and ended up on the top floor of the hospital.
As it was the early hours of the morning, most of the patients were asleep and the ward was dark.
We got placed in a 6 bay room and our bed was right in front of the nurse’s station.
In some ways the bed wasn’t needed as the next couple of hours were frantic.
The nurses were left with a list of jobs, one being, get a cannula in.
A few hours later a doctor appeared and hovered by the nurse’s desk, surveying the scene in front of her.
The scene of nurses trying to get lines in, Billy screaming, me saying enough was enough and the poor other patients just watching in horror from behind their sheets.
She came walking over with intent and closed the curtains to conceal the visual images from the other patients.
Then she moved the nurses out of the way and had a look at his hands and feet.
She commented ‘his feet and hands are cold’ and looked at the nurses who said nothing.
Then she looked at me and said ‘we need to get him warm and calm.’
So, I turned to the pram and got out a blanket.
She asked where the hospital lining had gone?
I replied, we haven’t been given any.
She turned and scowled at the nurses.
As one nurse scurried away, the lovely Italian doctor reappeared.
After hours of trying, he had managed to get through to the liver specialists.
At this point the liver specialist believed the fluid within Billy’s tummy was a leak from the Kasia operation.
He explained the specialist would like Billy to be transported back to them, so they could undertake a second operation.
He explained this could be tricky if they couldn’t secure a specialist transport ambulance crew.
So, plan B would be an operation within the local hospital with a surgeon over video call with the surgeon from the specialist liver team.
Either way the first job was, getting lines into Billy and put him to sleep.
This would help the team to manage his breathing for him.
I nodded.
He said ‘I think it would be nicer for everyone to get an anaesthetist in to put him to sleep before attempting any more lines’.
I continued to nod and stared at the floor, with floods of tears rolling down my face.
He reached over and put his hand on mine and said ‘I will be with you until you go.’
I looked up and smiled and I asked if he would look at Billy sore bottom from all the diarrhoea.
He nodded, after an examination and a trip to the medication room he came back with a pot of cream.
He passed it to me and said, ‘my mum used to make this for all the children in our family.’
On the way out, he closed the curtains and started to talk to the other female doctor from earlier.
After a few minutes of listening to the conversation, it became clear that this female doctor was the surgeon that had been tasked with the operation if moving Billy was not an option.
As the conversation got more in depth, the worry in her voice became more evident.
Then the words a parent never wants to hear emerged, I can’t remember the exact words, but I can remember her expressing that she didn’t want to do the operation.
After listening to this, I opened the curtains and said ‘if she wasn’t happy, I wouldn’t be happy either.’
They both looked at me, I flapped the curtain and said ‘they’re not sound proof, I heard everything.’
We all stood in silence for what felt like an eternity.
The Italian doctor half smiled and moved the conversation on with a ‘to do list.’
Right, he said ‘we need to get the anaesthetist team in to put him to sleep, put lines into Billy and make him comfortable and find a specialist transport team’.
He smiled and nodded at me, before he turned and moved away from the cubical.
By the time the golden morning sun had started to shine through the oversized glass windows, the energy of the team around Billy had changed.
The frantic attack had moved into a more focused and composed approach.
As Billy slept in an induced comma the team around him was forming and information started to trickle in about the very complicated mission that lay ahead.
By late morning we had a specialist transport team that consisted of 3 members, a surgeon, a specialist theatre nurse, and a specialist paramedic.
These 3-specialists visited one by one to get a visual on Billy, they were all as cool as a cucumber.
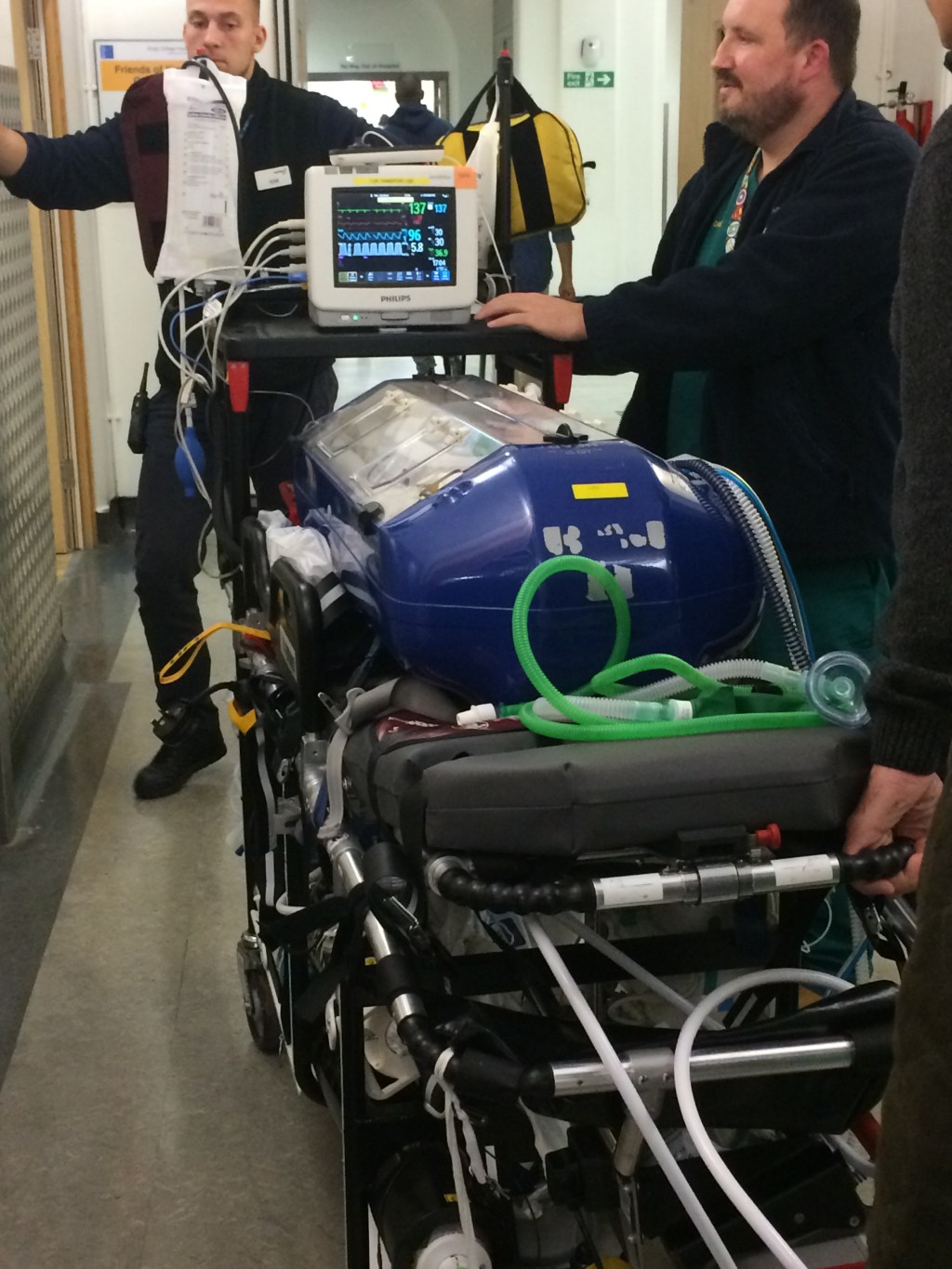
On the last visit they all emerged with a blue rectangular box strapped to a trolly.
The blue was bright and covered 5 sides, but the top had 2 see-through plastic doors.
The inside was small and padded, a hospital sheet had been draped over the inside to make it look more inviting.
The image was hard to compute, as on the one hand it looked like a coffin, but on the other hand it looked like a futuristic chamber.
As my brain was processing the image in front of me, the team continued to work.
As a team they lifted Billy slowly towards the box, one supporting his head as his arms and legs dangled limply from the sedation.
As the other 2, moved the oxygen tube and arranged the many cables.
Over these final preparations Alec, Billy’s father, arrived and was introduced to the team.
A couple of minutes later we started the long walk to the ambulance, Billy leading the congregation followed by the 3-specialist forming a triangle around the back of the trolly.
As we approached the lift and pushed the button, the emotions got the better of me.
The image of Billy’s bright blue coffin was to much and the thought we may lose him took over.
The specialist paramedic caught me and after a polite exchange of conversation, he said, ‘when I look worried, you can start to worry.’
The lift doors opened and we shuffled in and descended to the basement, before navigating the back of A&E into the ambulance bay.
As we stowed everything away there was one last question, the unthinkable, even if I asked you to guess, you would never guess right.
‘If Billy becomes unwell, we may have to stop and administer surgery,’ said the surgeon.
He continued ‘As there are only 3 of us, we would need one of you to help by holding the phone that would have the video link on it to the surgeons at Kings College Hospital’.
In my tired weary state, I just looked at Alec and before I could say anything, he said ‘I will do it.’
‘Great’ said the surgeon.
As we left the hospital the blue lights went on and the twists and turns started until we met the motorway.
After a couple of hours which seemed an eternity, the little window between the back and the front cab opened.
‘We are about 20 minutes out, hold on, the twists and turns will be back,’ said the paramedic.
Only a few minutes later, he spoke again, ‘there are road works ahead, I’m going to take an alternative route.’
‘Hold on, there is quite a lot of speed bumps this way’ he said.
As we ground to a halt, the doors quickly opened and Billy was prepped for his final trip to the surgeons, with us leading the way as the building was an unknown centre to the team.
As the doors opened on the lift on the top floor, there was a crowd of medics waiting for Billy.
The two teams merged around Billy’s bed that was being pushed towards the operating theatre.
Vital information was being exchanged and questions being asked.
As we reached the theatre doors, it was time to say our ‘good byes.’
The team opened the see-through plastic doors on the coffin for one last kiss on the forehead.
As we walked away there was a sigh of relief.
The knowing that Billy was in the best place to receive the best chance.
The feeling of, ‘we made it’ was real.


The next 12 days where a whirlwind.
The back-to-back operations had taken a great toil on Billy’s little unwell body.
To the point, he was still fragile on discharge.
But he was alive and we were thankful for that.


Remember you may not feel strong but you are
Love
The Rose-Tinted Mum