At times life throws you little bumps in the road, to remind you of where you are sitting in life at any given moment.
Sometimes these temporary setbacks appear to remind you of your past and the strength you have.
It also shows you how far you have come, or unearths areas you need to work towards.
Which allows you to fine-tune and reinforce your internal coping mechanisms.
But once they are refined you can take on the world.
One of the biggest challenges we had to adapt to when Billy was diagnosed with Biliary Atresia was blood taking.
We found out quite quickly, the sicker the child the more blood they wanted.
So over time Billy’s veins became weak and fragile and harder to use.
Which created an environment of endless attempts by highly skilled phlebotomist to find the much-needed blood.
The tension was clear within the medics that faced this unforgiving challenge.
Especially when your intentions are to help, but to do this you need to hurt the small being you are caring for.
The emotional wear was brutal, especially on us as parents, as we attended every attempt.
Once the element of surprise faded, Billy moved into a more watchful state.
The door became the enemy, the slightest sound would put Billy into high alert.
Later Billy was nicknamed rubberneck due to his sharp reactions.
His movement was intentional, he wanted eyes on the goods.
Threatening objects normally arrived in white plastic hospital trays and Billy communicated his dislike as soon as he saw them by waving his hands, crying and later saying no.
This defence mechanism would continue until he was able to identify the goods within their hands.
And determine if they were friend or foe.
Most often, Billy was on the money with the white plastic tray and would make it hard for medics to get near him to even look at the entry points.
Billy would wiggle his limb frantically to try and remove it from their grip, whilst he was pushing them away with the others.
This struggle needed to stop, so the doctors had the best chance of finding the precious internal source of information that aided their decision making.
Which gave us as parents one of the most difficult jobs, restraint.
Both Alec and I understood our job within the moment.
But by doing so we gained visual memories that will last a life time.
I will never forget his little face, looking at mine
Wide eyed and confused
As the floods of tears started to engulf his once defined blue eyes
The tears started to escape down his naïve face as his once helpful hands were swaddled tightly to prevent escape
But still allowing enough movement for wrestling to continue beneath the crisp white sheet
Except for the exposed limb that was protruding for examination
The cascade of sadness continued to roll rapidly down his cheeks
Soaking his clothes beneath his chin
The once soft cries grew into blood curdling screams
Communicating his distress
His once confused look, questioning the one he loves
Not knowing this act is for his own good
Forever sorry
Forever grateful for your forgiveness



After months of heart-breaking peripheral bloods from the hands, feet, the crucks of the arms and sometimes more unusual places like the side of the wrists.
It was agreed in early 2018 that this was not a reliable source of accessing bloods.
Billy’s head doctor had requested the support of the hospital board and his liver team to insert a central line.
A central line is a thin tube that is inserted into a large vein near the centre of the body. Which is accessible on the outside of the chest by a catheter tale with a connecter that can be attached to a single, double, or triple lumen.

After a little pushing back and forth, it was agreed.
We had a date set for early March 2018, but it snowed and many of the theatre roofs leaked, so Billy’s surgery was delayed for a couple of days.
Which created an inpatient snow day for the 3 of us.
So, once we got the ok by his medical team to leave the ward, we escaped.
For some much-needed fun before returning to find that the snow had prevented some staff being able to get home.
So, with much excitement, the staff had a sleep over within the communal areas of the wards.
Which brightened up ground hog day.


After months of torture, it was a relief to have a source of blood on tap.
By having this line, it gave a brighter outlook on the day, it made things more predictable and easier to manage.
In some ways, blood taking became a simple and effortless task.
And it was lovely to see overtime Billy’s watchfulness and high alert state starting to ease.
Which allowed Billy to enjoy life once again and trust all the adults around him.
After 6 months of bliss, Billy’s central line moved with catastrophic consequences.
Billy was admitted at Kings College Hospital at the time, for his life saving liver transplant.
In some ways we were just thankful that this came at the end of his stay and gave Billy much needed access for his operation.
Like most removals, there is always an element of healing that needs to be done before you can reinsert.
Which gave the team time to discuss and make plans for our next step.
Over the coming weeks whispers started to appear that Billy may not need a new line.
The theory being, he should be more stable and healthier with his new liver.
So, we all decided to put a new line on hold.
At first, I agreed with this decision, until the admissions continued.
We ended up in a predictable admissions routine.
One week in, one week out.
With constant infections, manly being chest infections and suspected cholangitis that would end in Billy spiking a temperature.
After transplant there are strict protocols to follow, one being fevers.
38.0 C or above the child needs to see a doctor and have bloods.
37.0- 37.9 C the child may have Calpol/ Paracetamol x 1 dose, but if the temperature persists for more than 12 hours, they must see a doctor and have bloods.
This normally ended in a 7 day admission for antibiotics.
This was relentless and hard work due to no reliable access.
Most admissions would end abruptly due to no access to give treatment.
Which meant Billy would return home still sick.
It felt that life couldn’t be lived, which was heart breaking after the year we had experienced up to transplant.
In April 2019, enough was enough and the local agreed to put in a temporary line in the form of a PICC, while they fought to get Billy a permanent line.
A PICC line is a peripherally inserted central catheter. A flexible line is inserted into a vein in the upper arm where it can be accessed by a lumen.

Unfortunately, it only lasted 2 months, to the despair of the medics.
Even that plans where in motion for a permanent line, it still was in its infancy.
Once again there was a divide amongst the professionals, if it was needed or not.
And it sat between the local hospital and the liver specialists.
Which was predictable, really considering the majority of Billy’s daily care was given by our local hospital.
It’s easy to make such decisions when you’re not the ones experiencing the daily hardships.
Over the coming months we continue to share evidence which highlighted the ineffective treatment programmes provided due to unreliable access.
This also included the emotional distress on Billy and the effect it could have on him long term.
For example, the effects these negative events would have on Billy’s willingness to attend hospital in later life.
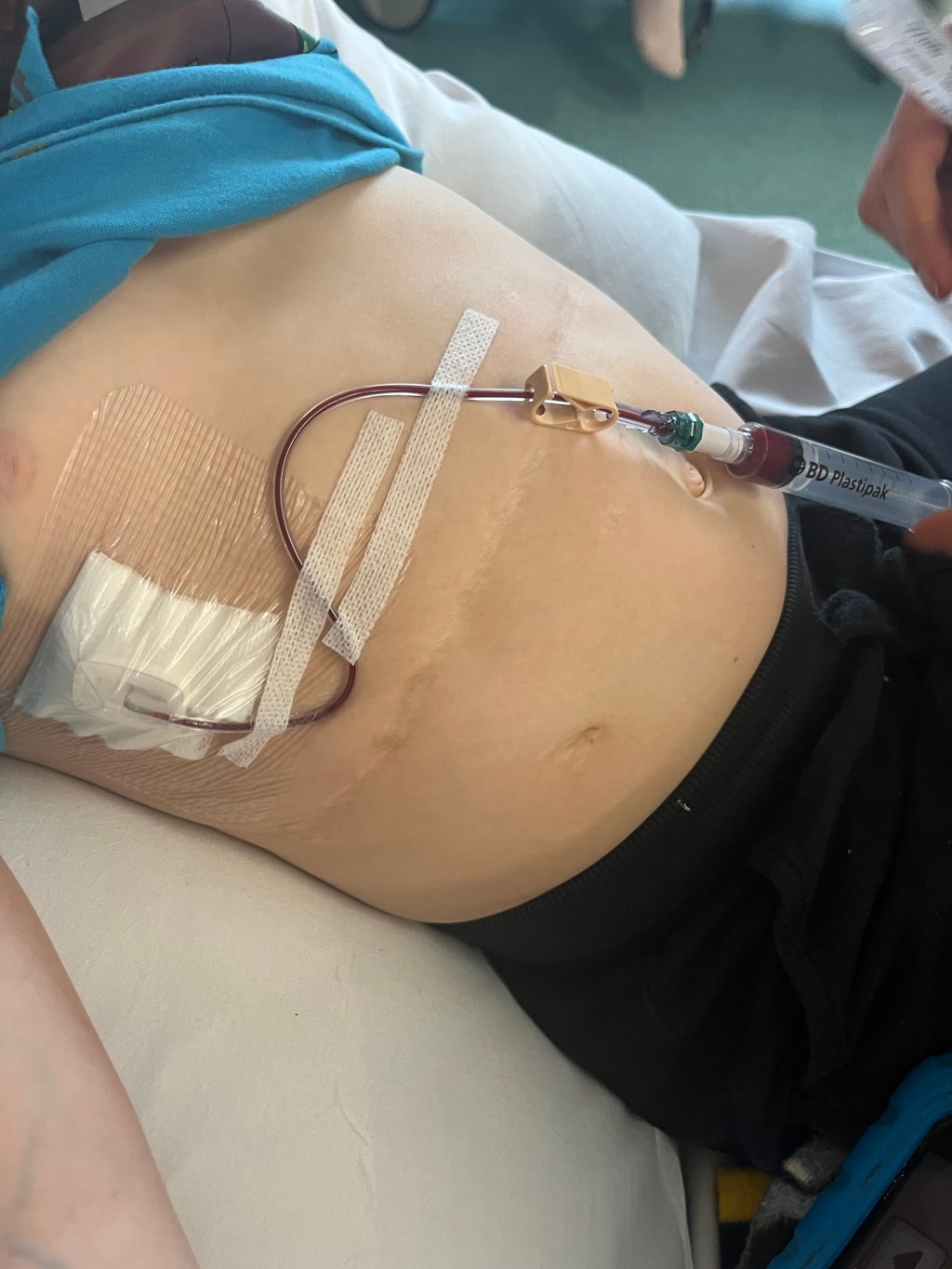
With a little bit of persistence Billy became the proud owner of a Port-a-cath in September 2019.
A Port-a-cath is very similar to a chest central line, except every thing is under the skin. A flexible tube is inserted into a vein and is then connected to a small, disc-shaped reservoir under the skin.

This line was chosen for Billy as a long-term solution, so he could still enjoy all activities that other young children do.
Like, any activity that would submerge Billy’s upper body in water.
So, when this line was compromised 2 weeks ago, you can probably understand my fear around losing it.
It started the week before February half term.
As usual Billy was booked in for monthly bloods and a line flush.
Line flush- is when a saline solution is put down the port-a-cath to clean the line, but also the nurse checks for blood by drawing blood back into the syringe before they continue to put the solution in.
The needle went in, a small amount of saline flush solution entered the line but, on the drawback, James couldn’t be found.
James- is the nickname Billy gave his blood; it is named after James the cheeky Tank engine from Thomas the Tank Engine. If you didn’t know James is bright red.

Over the next 30 minutes we fed Billy water, contorted his body into funny positions, added more saline flush in, all to help the line work.
But all our efforts where in vein.
After a conflab between the 3 of us, the Nurse, Billy and I, we decided to Heparin lock the line and take the needle out.
Heparin is a solution used to decrease the clotting ability of the blood within the line. Preventing harmful clots from forming in the blood vessels.
With the understanding we would all reconvene on the Friday to try again.
We all left with jobs to do in the meanwhile.
The Nurse would contact our local for advice on further action if we couldn’t find blood again.
For Billy to drink lots of water and work up a sweat on Friday morning.
And for me, don’t google search, relax and think of tranquil thoughts.
Friday came and we found a trickle of blood, not enough to take a discard or sample.
Discard blood is taken to reduce contamination and remove potential inhibitory substances.
So, plan B was actioned, a day at the Local with the unblocking solution.
So, after an early start, we prepared Billy with a needle and inserted the unblocking solution to dislodge the possible blood clot within his line.
And, I’m happy to say after 2 long hours of waiting we found James.
Remember you may not feel strong but you are
Love
The Rose-Tinted Mum
Keep up to date
@ The Rose Tinted Mum by subscribing to the News Letter to never miss a post.